Abstract
Background: Patients with COVID 19 disease have haemostatic dysfunction and are at higher risk of thrombotic complications. Although age and sex are a major risk factor for outcome. Even though the incidence of COVID 19 seems to be similar in both genders, men are at a higher risk of a worse outcome, with the odds up to 2.8 times higher than those for women. It is not known whether sex hormones contribute to this preposition. The real impact of sex hormone levels on the severity of COVID 19 remains to be demonstrated.
Objectives: We aimed to investigate the impact of variations in sex hormone levels on the hypercoagulability and severity of COVID 19 in women and men according to age.
Methods: 186 patients with symptomatic newly diagnosed Covid 19 were enrolled in the study. Specially we included postmenaupausal women (>50 years) and age matched men. Participants were divided into two groups: moderate Covid-19 (ARDS) and severe Covid-19. The control group consisted of 60 healthy individuals, with the same age as patients. Biomarkers of hypercoagulability and endothelial cell activation: Procoagulant phospholipid (PPL) TFPI, D-Dimer, Soluble thrombomodulin , Tissue factor activity, Thrombin generation (TG) with the Calibrated Automated Thrombogram (CAT) were all measured with assays were from Diagnostica Stago, Asnières, France. Total testosterone, estradiol, and progesterone were measured by ELISA method (Abcam, France). IL-6, Complement C3a and C5a by Human IL-6 ELISA kit, ThermoFisher (Scientific Asnieres-sur-Seine, France). The Upper Normal Limit (UNL) and the Lower Normal Limit (LNL) for each studied biomarker were defined in the control group as follows: UNL= mean + 2 standard deviation (SD), and LNL: = mean - 2 SD.
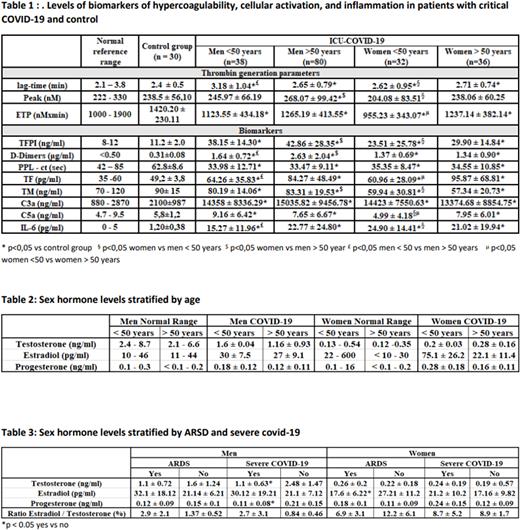
Results: The levels of biomarkers of hypercoagulability, endothelial cell activation and inflammation in patients and controls are reported in Table 1. Thrombogram was marked by significantly prolonged lag time, prolonged time to peak and decreased ETP compared to the control group. The comparison between females and males showed that the lag-time was over the UNL in 18% of men over 50 years versus 8% in men under 50 years, and in 10% and 0% of women respectively. ETP values were below the LNL in 82% of men over 50 years versus 63% for men under 50 years and in 54% and 92% for women respectively. In the same way, the peak of thrombin was over the UNL in 39% and 15% for men over 50 and men under 50 versus 12% and 0% for women respectively. The TFPI were over the UNL in 99% of men over 50 years and in 84% of men under 50 years versus 91% and 87% for women respectively. D-Di increased in 88% of patients under or over 50 years independently of the group. The PPL were shorter than the LNL in 90 % and 80% of men over and under 50 years respectively, and for women in 86% and 77% respectively. The levels of TM were significantly lower in women for the 2 groups in comparison with men over or under 50 years. The levels of C3a, were above the UNL in 86%, and 63% for men over and under 50 years respectively and in 55% and 87% of women over and under 50 years respectively. The testosterone levels in males both younger and older than 50 years were significatively below the lower limit of the normal range of each age group. The estradiol levels were in normal range for women but significantly increased men (Table2). Stratification by the severity of COVID-19 showed that the testosterone levels were significantly lower in men who developed ARDS or severe COVID-19 than in those who did not (p>0.05). In men, the estradiol levels were significantly increased but the difference was not significant between those with severe or mild COVID-19. Males who developed severe COVID-19 had a lower progesterone level. No statistically significant difference in testosterone or progesterone levels were found in the women compared to normal range, the estradiol level was lower in females with ARDS (Table 3.)Relationship analysis of sex hormones with markers of immune activation, testosterone levels and estradiol/testosterone were correlated with, IL-6, fibrinogen, and D-Di.
Conclusion: Our study highlights that disturbance in circulating sex hormone levels is a hallmark of critical COVID-19 in males and reinforces the concept that determination of testosterone and E2/T ratio in association with biomarkers of hypercoagulability upon diagnosis might lead to an a accurate risk assessment tool for prompt identification of patients at high risk of COVID-19 worsening.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.